Hot topics – Rethinking healthcare education, training and skills to enable AI adoption
Key themes and emerging challenges: lifelong learning and the importance of cross-sector knowledge sharing
With increased use of AI tools in healthcare, there is a need to ensure healthcare professionals (HCPs) are equipped with the digital literacy and critical thinking skills needed to navigate and use them effectively. But with over a third of healthcare providers citing education and skills as the biggest barrier to adopting AI, it seems there is still a long way to go.1
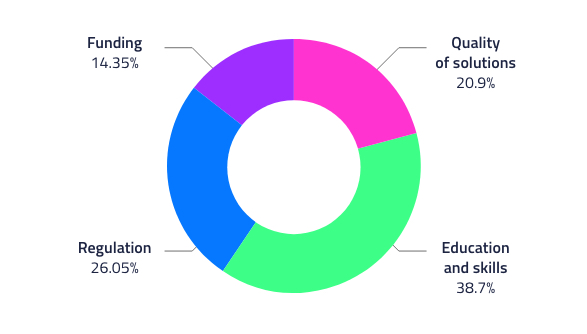
EIT Health online poll: What needs to change to encourage AI adoption in healthcare? (2,009 responses)
AI has the potential to take on arduous, data-heavy and time-consuming admin tasks. It can provide major benefits, such as comparing a patient’s scan with millions of images on a database to aid the treatment decision-making process – a task that is impossible for humans to carry out. In turn, this frees up time for direct patient care – the sort that cannot be replaced by AI.
However, for patients to reap the full benefits of AI solutions, clinicians need more than a basic understanding of what tools are available, how they are best applied, and how to interpret their outputs.
AI education is required across every layer of society
The seven Round Table Meetings were attended by key stakeholders who play a role in developing and implementing AI approaches at scale within existing national healthcare systems. Participants across the Round Tables were in agreement – it is essential AI is included in the medical curriculum from the very beginning, as well as in continuing medical education programmes and for all healthcare workers. This is because, whilst data scientists will be critical to the adoption and operation of AI systems, on-the-ground clinicians require strong data science skills to enable them to work with the technology daily. Current undergraduate education in this area must go further, and postgraduate courses must help develop the skillsets into specialisms.
Key insights – Poland
Most AI professionals are graduates of computer science, mathematics, IT, engineering, physics, mechatronics and robotics – there is a definite gap in the education of medical students
Research centres, universities and healthcare units must collaborate to enable access to anonymised data that can be used for education, for example to be used for students’ research as part of a postgraduate study. Having such data to work with and conduct research on will enable HCPs and students who are studying AI to gain a deeper understanding of how it works and the outputs it can generate
I think that anyone who is going into a health profession now needs to have an understanding of what data science is [and] what AI can bring. And I do believe we will start putting data scientists into hospitals.
Yet, education doesn’t stop here. The digitisation of healthcare requires training not just for HCPs, but for patients and citizens too. AI is ultimately a patient-focused innovation and gaining the trust of patients is critical to its widespread uptake. AI cannot exist without data and in healthcare, this is complex and often sensitive patient data. Whilst there are major barriers due to security, trust and consent, helping patients to understand the benefits of AI may make inroads to overcoming these challenges.
Activating AI education for HCPs
Across the seven Round Table Meetings, participants highlighted that, whilst the education movement needs to be holistic, it has to be driven by clinical leaders who will prioritise the education of their teams, for example by affording HCPs the time and motivating them to take educational courses or engage in on-the-job training. Leaders are also in the position to enable the cross-fertilisation of innovative ideas focused on the use of AI across their teams. Furthermore, to incentivise ongoing learning and to acknowledge that many HCPs have limited time, education needs to be diverse – learning opportunities should take place online, as part of secondments or ‘gap years’ as well as formal and on-the-job training.

Key insights – Ireland
Participants in Ireland highlighted that academic institutions can be slow to adopt new curricula and there can be reluctance to change an already intensive medical school programme. However, the COVID-19 pandemic has highlighted that learning methods can, and indeed sometimes have to, change and this process can be accelerated if needed. Examples of best practice include:
The University of Limerick has developed and implemented an online Masters course in AI in under a year
Imperial College and Great Ormond Street Hospital in London both have programmes where data scientists doing PhDs can work in tandem with clinical teams
Participants agreed that collaboration between innovators, industry, academia and HCPs will create optimal educational opportunities. Such cross-sector knowledge sharing will create a medical workforce equipped to handle modern digital healthcare systems. However, whilst education can be driven at country-level, EU support would be helpful in terms of standardising the curriculum of educational programmes, or providing incentives to member states to offer education on AI and data science.
To enable widespread adoption of AI, it has to reach the medical front-line and its benefits must be undoubtedly clear. The way to make this happen, as highlighted by the Round Table participants, is through education. Whilst there are many options for the roll-out of education and training, there is undoubtedly the expertise and drive to make it happen.
Do you agree with the key points raised at the Round Table Meetings? Do you have insight into how best to integrate training on AI into medical curricula? Let us know and continue the conversation on our social media channels. Tag @EITHealth on Twitter and share your thoughts using the hashtag #EITHealthAI
1 EIT Health online poll